Home » Archives for February 2012
Tuesday, February 28, 2012
Sunday, February 26, 2012
Saturday, February 25, 2012
Delayed Puberty
Definition:
- Absence of breast development by the age 14 years
- If more than 3 years elapsed between the onset of breast development & menarche
- Absence of menses by the age of 16 years in presence of good secondary sex characters
Puberty
Definition: It is the period of life having a physiological changes proceeds over an average 4-5 years after initiated during which-
Theories of Pubertal Initiation:
The exact cause of the initiation of pubertal changes is not fully understood
Pubertal Changes:
The sequence of events occurring at the time of puberty:
Pubertal Stages: Tanner's Classification:
Tanner's staging is a system based on the orderly, progressive development of breast (thelarche) & pubic hair in females.
Factors Affecting the Age of Menarche:
Age of menarche varies from society to society and in Egypt, it usually occurs around 12.5 years. Many factors can affect the age of menarche such as:
- Sex character develop
- Sex organ mature
- Reproductive capacity attained- maturation of hypothalamus, pituitary and gonads
Adolescence - Includes the physiologic, social, behavioral & personal independence leading to the development of adult identity. It is broader term than puberty.
Theories of Pubertal Initiation:
The exact cause of the initiation of pubertal changes is not fully understood
- Gonadostat theory
- Critical weight & body fat mass
- Onset of adrenal activity
- Sleep mechanism
- Central nervous system maturation
Pubertal Changes:
The sequence of events occurring at the time of puberty:
- Thelarche (breast development)- breast bud appears at age 9-11, sign of ovarian production & completed over 3 years.
- Adrenarche (maturation of adrenal gland)- production of 17 ketosteroids, DHEA & DHEAS, development of pubic (pubarche) and axillary hairs, follows after thelarche but can be first sign in 20% of girls.
- Growth spurt- 3 phases; 5cm/year of minimum growth velocity, 8.5cm/year of peak height velocity & stage of decrease velocity.
- Menarche (spontaneous first menstrual flow)
- Anatomical maturation of the genital tract
- Behavioral changes and psychic maturation
Pubertal Stages: Tanner's Classification:
Tanner's staging is a system based on the orderly, progressive development of breast (thelarche) & pubic hair in females.
Stages of pubic hair growth | Stages of breast development | |
No pubic hair. | No breast tissue (elevation of papilla only). | Stage 1 |
Sparse, long pigmented hair along the labia major. | Breast bud. | Stage 2 |
Darkening, coarsening, curling of hair which extends upwards and laterally. | Enlargement of breast and areola without separation. | Stage 3 |
Hair of adult consistency limited to the mons. | Areola and nipple form a mound on top of underlying breast tissue. | Stage 4 |
Hairs spread to the medial aspect of the thighs. | Adult configuration with areola and breast having smooth contour. | Stage 5 |
 |
| Click on the picture to enlarge |
 |
| Click on the picture to enlarge |
Factors Affecting the Age of Menarche:
Age of menarche varies from society to society and in Egypt, it usually occurs around 12.5 years. Many factors can affect the age of menarche such as:
- Socio-economic factors
- Environmental factors
- Racial & geographical factors
- Medial & endocrinological diseases- blindness, deafness, epilepsy, obesity & diabetes (all accelerates puberty development)
Gynecology Book
Contents
- Anatomy of the Female Tract
- Embryology of the Female Genital Tract
- Gynecology Case Taking
- History Taking- (Personal History, Chief Complaint, Menstrual history, Obstetric history, Past History, Family History, Present History)
- Clinical Examination- (General examination, Abdominal Examination)
- Investigation
- Diagnosis
- Reproductive Endocrinology & Infertility
- Gynecology Endocrinology
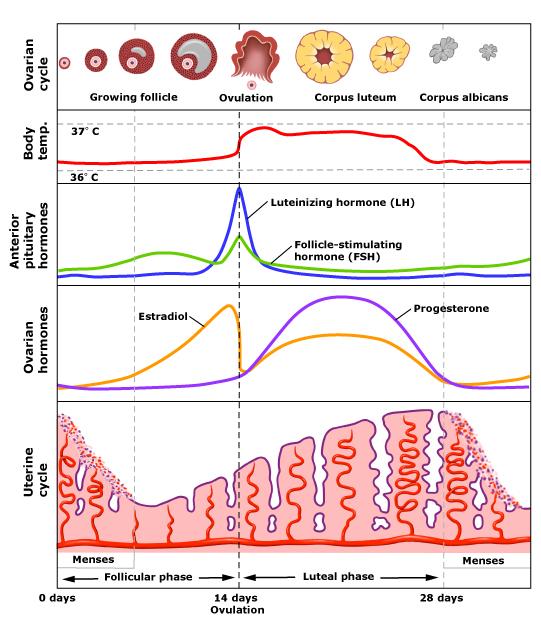
- Physiology of the Menstrual Cycle
- Puberty, Delayed Puberty & Precocious Puberty
- Menopause
- Menstruation Related Symptoms
- Amenorrhea
- Abnormal Bleeding from Genital tract
- Sexuality & Sexual Dysfunctions
- Female Genital Cutting (Mutilation)
- Infertility
- Ovulation Dysfunction
- Virilization in Female
- Reproductive Tract Infections
- Sexual Transmitted Disease (STD)
- Pelvic Inflammatory Disease (PID)
- Infection of Female Genital Tract
- Female Genital Tuberculosis
- Bilharziasis of Female Genital Tract
- Leukorrhea
- Pruritus Vulvae
- Displacements of Female Genital Tract
- Traumatic Lesions & Urogynecology
- Uterine Fibroid
- Endometriosis
- Adenomyosis
- Cysts & Swellings Related to Vulva
- Chronic Vulval Dystrophies (Dermatoses)
- Gynecologic Oncology
- Contraception
- Breast Evaluation for the Gynecologist
- Benign Breast Disease (History, Clinical Examination)
- Breast Cancer (History, Clinical Examination)
Tuesday, February 21, 2012
Partograph
 |
| Click at the picture to enlarge |
- A partograph is a graphical record of the observations made of a women in labour
- For progress of labour and salient conditions of the mother and fetus
- It was developed and extensively tested by WHO
- Friedman’s partogram devised in 1954 was based on observations of cervical dilatation and fetal station against time elapsed in hours from onset of labour. The time onset of labour was based on the patient’s subjective perception of her contractility. Plotting cervical dilatation against time yielded the typical sigmoid or ‘S’ shaped curve station against time gave rise to hyperbolic curve.
- The partograph can be used by health workers with adequate training in midwifery who are able to:
o Observe and conduct normal labour and delivery
o Perform vaginal examination in labour and assess cervical dilatation accurately
o Plot cervical dilatation accurately on a graph against time
- There is no place for partograph in deliveries at home conducted by attendants other than those trained in midwifery
- Whether used in health centers or in hospitals, the partograph must be accompanied by a partogram of training in its use and by appropriate supervision and follow up
Objectives:
- Early detection of abnormal progress of a labour
- Prevention of prolonged labour
- Recognize cephalopelvic disproportion long before obstructed labour
- Assist in early decision on transfer, augmentation or termination of labour
- Increase the quality and regularity of all observations of mother and fetus
- Early recognition of maternal or fetal problems
- The partograph can be highly effective in reducing complications from prolonged labour for the mother (postpartum hemorrhage, sepsis, uterine rupture and its sequelae) and for the newborn (death, anoxia, infections, etc)
Functions:
- The partograph is designed for use in all maternity settings, but has a different level of function at different levels of health care
- In health center, the partograph’s critical function is to give early warning if labour is likely to be prolonged and to indicate that the woman should be transferred to hospital (ALERT LINE Function)
- In hospital settings, moving to the right of alert line serves as warning for extra vigilance, but the action line is the critical point at which specific management decisions must be made
- Other observations on the progress of labour are also recorded on the partograph and are essential features in management of labour
Components:
The partograph can be divided into three parts:
- Part 1: Fetal Condition (top)
- Part 2: Progress of labour (middle)
- Part 3: Maternal Condition (bottom)
Outcomes:
[A] Part 1: Fetal Condition
This part of the graph is used to monitor and assess fetal condition:
- Fetal heart rate
- Membranes and liquor
- Moulding of the fetal skull bones
[B] Part 2: Progress of Labour
This section of the graph has its central feature; a graph of cervical dilatation against time, use to assess the following:
- Cervical dilatation
- Descent of fetal head
- Fetal position
- Uterine contractions
It is divided into a latent phase and active phase:
Latent phase: | Active phase: |
It starts from onset of labour until the cervix reaches 3 cm dilatation | Once 3 cm dilatation reached, labour enters the active phase |
Lasts 8 hours or less | The cervix should dilate at a rate of 1 cm/h or faster |
Contractions at least 2/10 min | Contractions at least 3/10 min |
Each lasting < 20 seconds | Each lasting <40 seconds |
Alert Line (health facility line)
- The alert line drawn from 3 cm dilatation represents the rate of dilatation of 1 cm/hour
- Moving to the right or the alert line means referral to hospital for extra vigilance
Action Line (hospital facility line)
- The action line drawn 4 hours to the right of the alert line and parallel to it
- This is critical line at which specific management decisions must be made at the hospital
[C] Part 3: Maternal Condition
- Name / DOB / Gestation
- Medical / Obstetrical issues
- Assess maternal condition regularly by monitoring:
o Drugs, IV fluids 7 oxytocin, if labour is augmented
o Pulse, blood pressure
o Temperature
o Urine volume, analysis for protein & acetone
jj
Saturday, February 18, 2012
Genital System Changes During Pregnancy
- Uterus
a) Body of uterus -
b) Isthmus - is transformed into the lower uterine segment.
 |
| Upper uterine changes during pregnancy (click at the image to enlarge) |
 |
| Lower uterine changes during pregnancy (click at the image to enlarge) |
- Cervix
- Hypertrophy & softening of the cervix
- Hypertrophy of cervical mucosa
- Increased vascularity of the cervix
- Cervical mucous plug closes the cervical canal due to excess cervical secretion, it is discharged as bloody show with the onset of labor
- Rearragement of collagen fibers
- Vagina & vulva
- Hypertrophy & softening
- Varicose veins of the vulva (Kluge's sign)
- Blue or violet discoloration of the vulva (Chadwick's sign)
- Vaginal pH is acidic (3.5 - 6) due to increased production of lactic acid by lactobacilli
- Vaginal cytology show increased small intermediate cells under the effect of progesterone
- Ovary
- Genital System Changes
- Breast Changes
- Cardiovascular Changes
- Respiratory Changes
- Gastrointestinal Changes
- Liver & Gall Bladder Changes
- Urinary Changes
- Skin Changes
- Skeletal Changes
- Nervous System Changes
- Metabolic Changes
- Endocrinal Changes
- Immune System Changes
Friday, February 17, 2012
Scapula
Posterior View
.png) |
| Shoulder girdle & thoracic cage |
Definition: scapula is a flat bone that connects the trunk to the upper limb. It is the posterior bone of shoulder girdle. It is also known as shoulder blade.
Shape: triangular in outline.
Site: lies on the postero-lateral aspect of the chest wall extending from the 2nd to 7th rib.
Side determination:
- Glenoid cavity: is directed laterally & upwards.
- Spine is directed backwards.
- Subscapular fossa: is directed fowards.
 |
| Posterior, anterior & lateral sides of scapula |
General features: It is consist of 2 surfaces, 3 angles, 3 borders, 3 processes
- Surfaces:
Costal (anterior) surface | Dorsal (posterior) surface |
- It is directed forwards & medially - Facing the ribs - It carries subscapular fossa | - It is directed backwards & laterally - Palpated from back - Spinous process, divides it into two fossae: infraspinous fossa & supraspinous fossa |
- Angles:
Superior angle | Lateral angle (head) | Inferior angle (apex) |
- Thin, smooth & rounded - Right angle - Between superior & medial borders - Opposite the 2nd rib | - Thickest part of the bone - Glenoid cavity - Articulate with head of humerus - Supra & infraglenoid tubercles | - Thick & rough - Acute angle - Between medial & lateral borders - Opposite the 7th rib |
- Borders:
Superior border | Lateral (axillary) border | Medial (vertebral) border |
- Thinnest & shortest - Extend from the superior angle to coracoids process - Near the root of coracoids process, there is suprascapular notch | - Thickest - Extend from the glenoid cavity to the inferior angle - At the upper end, there is infraglenoid tubercle | - Average thickness & longest - Extend from the superior angle to the inferior angle - Presents anterior lip, posterior lip & an intermediate narrow area |
- Processes:
| Spinous process | Acromion process | Coracoid process |
| - A triangular plate of bone - Divides the dorsal surface into 2 fossae - It has 2 ends: § Lateral end- continuous with acromion process § Medial end- forms the root of the spine - It has 2 surfaces: § Upper surface § Lower surface - It has 3 borders: § Anterior border- attached to scapula § Posterior border- free, subcutaneous (crest of spine), has upper &lower lips § Lateral border- free, bounds the spinoglenoid notch | - A projecting forwards from the lateral end of the spine making right angle - It has 2 surfaces: § Upper surface § Lower surface - It has 2 borders: § Medial border- continuous with upper lip of crest of spine, carries small articular facet for articulation with clavicle (acromioclavicular joint) § Lateral border- continuous with lower lip of the crest of spine at the acromial angle | - A projection from the upper border of the head (glenoid cavity - Directed fowards & slightly laterally - Root of process is related medially to the supraglenoid tubercle & laterally to the suprascapular notch - It has 2 surfaces: § Upper surface- carries a rough area for muscle attachment § Lower surface - It has 2 borders: § Medial border § Lateral border |
.jpg) |
| Anterior surface of scapula (click at the image to enlarge) |
 |
| Posterior surface of scapula (click at the image to enlarge) |
.jpg) |
| Lateral border of scapula (click at the image to enlarge) |
Thursday, February 16, 2012
Hazard of Smoking to the Individual, Family & Environment
Smoking is associated with significant morbidity and mortality. Smoking still remains one of the leading cause of preventable death. Smoking has the dubious distinction of affecting all the systems from head to foot. Citizens of western countries no longer regard smoking as a good option to relieve their stress. Numerous universities worldwide do not allow their students to smoke in the campus.
General facts about smoking:
- About 111, 000 people die every year due to smoking or passive smoking.
- One person dies every 5 minutes from smoking related diseases.
- The NHS spend over four hundreds million pounds each year on treating smoking related illness.
- Cigarettes and other smoking materials are a very common cause of fires.
- Smoking materials account for almost 240 deaths every year.
- Out of 6, 600 fires 40% are cause by smokers- thats 2, 640 fires!
How smoking ruin the body:
- Heart disease- nicotine raises blood pressure making the heart work harder therefore it need more oxygen which is cut down from carbon monoxide from getting to the heart. This cause severe heart attacks.
- Lung cancer- this start with the smokers cough producing lots of phlegm. Chest infection and bronchitis begins causing the lungs to be destroyed.
How does smoking affect non-smokers:
- Non smokers can suffer from passive smoking.
- Non smokers can suffer from sore eyes, sneezing, runny nose, headaches, coughing, wheezing and hoarseness all due to other people's smokes
- Children of smokers have a very high risk of getting bronchitis, pneumonia and other chest infections.
- Asthmatic have a high risk of getting attacks due to other people's smoke.
- Non smokers have a high risk of getting lung cancer due to other people's smoke.
How the environment affect the environment:
- Each cigarette manufacturing machines uses 4 miles of paper per hour which could be used instead for many other important things.
- Tobacco is the most widely grown non-food crop in 120 countries therefore less land is available for food crop. Between 10 to 20 million people could be fed if food crop was grown in its place.
- Burning tobacco is the main source of indoor pollution in the developed world as it contains over 4,000 dangerous chemicals.
- One whole tree is needed to cure the tobacco for 300 cigarettes.
- Cigarette smoke generates contains two of the main gases related to the greenhouse effect they are carbon dioxide and methane.
- If smoker smoked a packet of cigarettes a day, the habits would cost around $1800 per year. Wouldn't they rather do something fun or beneficial with that money, like donate to the orphan.
- A broken leg of a smoker takes 80% longer to heal than a nonsmoker (276 days compared to 146).
- Secondhand smoke cause 3,000 causes of lung cancer in nonsmokers each year.
Chief Complaint
- The 1st complaint in any obstetric case should be cessation of menstruation since the last normal menstrual period (LNMP).
- This is followed by the main complaint (s) that brings the patient to hospital.
- Use patient own words
- Arranged in chronologically if the complaint is more than one.
Obstetric History:
Past History
Family History
Present history
Menstrual History
The items of menstrual history include the following items in sequence:
- [1] Menarche- it is the 1st menses in the woman's life. Normal age is between 9-16.
Precocious puberty: earlier than 9 years old
Delayed puberty: later than 16 years old
- [2] Cycle rhythm- whether the menses occur in regular or irregular period of time.
- [3] Cycle length- it is the duration from 1st day to the next 1st day of menses cycle. Normal cycle length ranges from 21 to 35 days.
<21 days - polymenorrhea
>35 days - oligomenorrhea
- [4] Duration of menstrual flow- It is the period of time during which the menstrual blood flow through the vagina. Normal duration of menstrual flow ranges from 2-7 days.
Menorrhagia: prolonged >7 days and/or 80cc occurring at regular intervals = hypermenorrhoea
Metrorrhagia: irregular uterine bleeding not related to menstruation
Menometrorrhagia: prolonged uterine bleeding occurring at irregular intervals
Polymenorrhagia: frequent heavy/ prolonged menstruation
Postmenopausal bleeding: irregular vaginal bleeding following menopausal cessation of menstruation by 1 year
Intermenstrual bleeding: irregular vaginal bleeding in between regular normal menstruation = breakthrough bleeding
Contact bleeding: irregular vaginal bleeding following tissue contact (examination/intercourse)
- [5] Character of flow- it is regarding the amount, colour and odour of the blood. Normal amount is not more than 80 ml of the total volume. Normal colour of mense blood is dark red.
Excessive flow- indicated by present of clots
Bright red- may indicate excessive flow especially if associated with clots
Polymenorrhea: frequent menstruation occurring at regular intervals (<21 days)
Oligomenorrhoea: infrequent menstruation varying between 35 days and 6 months
Hypomenorrhoea: scanty regular menstruation (<20 ml)
Amenorrhoea: absence of menses for 3 successive regular cycles or 6 months
- [6] Dysmenorrhea- It is pain related to menses. It is severe enough to prevent the woman from doing her daily activities. Dysmenorrhea may be primary or secondary. The tolerable pain at menses is called 'menstrual molimina'.
Primary (spasmodic) dysmenorrhoea
Secondary (congestive) dysmenorrhoea
Special types of dysmenorrhoea
- [7] Intermenstrual Period (IMP)- It is the period from the last day of flow to the next 1st day of flow. Abnormal pain, bleeding or discharge may be presence or absence.
Normally ovulation may cause pain (Mittleschmerz's pain), bleeding (ovulation spotting) or increase of vaginal discharge (ovulation cascade).
- [8] Last Normal Menstrual Period (LNMP)- The 1st day of the last normal menstrual period should be asked for. To certain that the last menstrual period was normal it should fulfill the following criteria:
- It should be normal characters
- It should be preceded by 3 consecutive normal cycles
- It should not be preceded by the use of hormonal contraceptive
NB- The expected date of delivery (EDD) is calculated & mentioned before.
- [9] Current use of contraceptive- It should be mentioned here if it is currently used. The type of contraceptive method and the duration of its use should be asked.
Subscribe to:
Comments (Atom)



.png)